A concussion is an injury to the brain. It affects the way a person may think and remember things and can cause a variety of symptoms.
This webpage contains the full concussion guide for adults 65+. If you prefer a printable PDF, download the PDF version of the guide below.
Concussion Guide for Adults 65+ (2025)
How concussions happen
Any blow to the head, face or neck can cause a concussion. A concussion can also be caused by a blow (sudden movement) to the body that causes the brain to move rapidly inside the skull.
Falls are the No. 1 cause of concussions for seniors in Canada. Other common causes include car crashes, being hit in the head with an object, hitting your head on something and violence.
Signs and symptoms of a concussion
You do not need to be knocked out (black out or lose consciousness) to have had a concussion. If you have a concussion, you may have one or more of the following symptoms:
Cognitive (thinking) symptoms:

- Changes to your memory
- Having trouble concentrating
- Feeling “in a fog”
Physical symptoms:

- Headache or pressure in your head
- Dizziness
- Changes to your balance
- Nausea or vomiting
- Feeling more tired or having low energy
- Sensitivity to noise or light
- Ringing in your ears
- Changes to your vision (blurry or fuzzy)
Other symptoms:
- More nervous, anxious or irritable than usual
- Changes in sleep patterns (sleeping more or less)
It is helpful to think of symptoms as changes to how you typically think and feel. Some symptoms of concussion are similar to symptoms of other conditions. Consult with a healthcare professional who is familiar with your health status and consider bringing a trusted caregiver, family member or friend who can help describe any changes in your health, wellbeing, emotions and the way you are able to do things.
When to get emergency help
Get medical help immediately if you notice any of these “red flag” symptoms. They may mean you have an even more serious injury:

- Neck pain or tenderness
- Double vision
- Weakness or tingling in arms or legs
- Severe or increasing headache
- Seizure or convulsion
- Loss of consciousness (knocked out or blacked out)
- Deteriorating conscious state
- Vomiting more than once
- Increasingly restless, agitated or combative
- Growing confusion
What to do if you might have a concussion
It is important to always tell a healthcare professional, family member or friend you trust if you have fallen or believe you have sustained a head injury, such as a concussion. Anyone with a possible head injury should be seen by a doctor or nurse practitioner as soon as possible.
If you are taking a blood thinner, it is especially important to seek medical attention right away after a possible head injury. You can have more bleeding if you are taking this type of medication.
Typically, you will be asked about what happened and your symptoms, and have a neurological assessment (e.g., checking your balance and eye movement). Concussions cannot be seen on routine X-rays, CT scans or MRIs. However, if you are 65+, your healthcare provider may order a CT scan to rule out intracranial bleeding (bleeding in the brain). Adults 65+ are at risk of intracranial bleeding from minor head injuries.
Managing and recovering from a concussion

Concussion healing times vary, but it is common for symptoms to last longer for adults 65+ compared to other age groups. Your symptoms may last for weeks or months.
Work closely with your healthcare professional(s) to support and tailor your concussion management and recovery. They should:
- Consider factors that could impact your recovery (such as pre-existing conditions and medications you are taking).
- Provide guidance on returning to activities, such as driving, working or volunteering and physical activity.
- Refer you, if needed, to other health-care specialists who can support your recovery, such as a physiotherapist, occupational therapist, optometrist, audiologist, geriatrician and/or psychologist. The type of professionals involved in your care will depend on your individual symptoms.
If your symptoms do not improve or last longer than four weeks, ask to be referred to a healthcare professional or team with expertise in the management of concussion for seniors.
Getting back to regular activities after a concussion

You don’t need to be symptom-free to begin returning to activities you enjoy. In fact, resuming cognitive activities (e.g., reading, general interest courses) and physical activities (e.g., walking, fitness classes) help your brain recover. The key is to take a gradual approach: add activities back in a bit at a time and be aware of how they make you feel.
Here are some general tips for returning to activities. Please note: This information does not replace guidance from your healthcare professional(s):
- For the first 24 to 48 hours after your injury, you can do activities of daily living, such as preparing meals, hygiene, spending time with family or friends, and moving around your home. Try to get proper sleep at night and take time to rest during the day. Minimize time using screens, such as a TV or computer.
- Do not drive in the first 24 to 48 hours if you are experiencing concussion symptoms. Talk to your doctor about when it is safe to drive again.
- After 24 to 48 hours, start adding activities that, for you, do not require a lot of effort. Examples might be going for a walk, reading, playing cards, doing a puzzle, listening to the radio or a podcast, or cooking. Take breaks as needed.
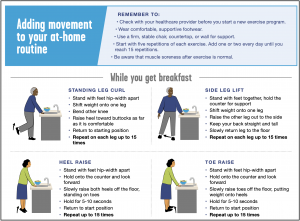
- Increase the amount of time and/or effort you spend on activities. Start adding more physical movement that is appropriate for you, such as stretching, walking, exercises, swimming, dancing or gardening.
- If you work or volunteer, gradually resume these activities by trying a shorter shift with breaks and building up from there. You might need some supports at first, such as being able to wear a hat or sunglasses to help with light sensitivity or having more time to complete tasks.
As you resume activities, it’s common for concussion symptoms to worsen briefly and mildly. If your symptoms feel much worse or worsen for more than an hour, stop the activity and try again the next day. See your primary care provider if your symptoms continue to worsen.
Note: If you participate in any activities that have risk of falls, contact or head impact, consult with your primary care provider before returning to these activities. Resuming these activities before full recovery from concussion can put you at higher risk of sustaining another concussion, with symptoms that may be more severe and last longer.
Prioritize your wellbeing
While you are recovering from a concussion:
- Pace yourself: Prioritize activities and take breaks as needed
- Practice good sleep habits, such as going to bed the same time every night
- Stay hydrated by drinking water throughout the day
- Eat nutritious foods such as vegetables, fruits, whole grains and foods that are a good source of protein and Omega-3 fatty acids such as fish and nuts
- Add movement and physical activities you enjoy into your day
- Stay in touch with others, such as family, friends, neighbours and others in your community
Preventing falls is important for your health
Some proven ways to prevent falls are:
- Exercises that build balance, strength and flexibility
- Managing your medications and reviewing them regularly with your pharmacist or doctor. Some medications may make you dizzy and increase your risk of falling.
- Using a cane or other mobility aid if needed.
- At home, putting hand rails along stairs and safety grab bars in the bathroom
Ask your healthcare professional for more information about preventing falls based on your individual risk.
Resources
Below are resources and tools that may be helpful to you. This is not a complete list. You may find local resources and services through your public health unit, hospital, medical clinic, brain injury association or other community organization.